IMPORTANT SAFETY INFORMATION
WARNINGS: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS and SUICIDAL THOUGHTS AND BEHAVIORS
- Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. VRAYLAR is not approved for treatment of patients with dementia-related psychosis.
- Antidepressants increased the risk of suicidal thoughts and behaviors in pediatric and young adult patients in short-term studies. Closely monitor antidepressant-treated patients for clinical worsening, and for emergence of suicidal thoughts and behaviors.
Contraindication: VRAYLAR is contraindicated in patients with known hypersensitivity. Reactions have included rash, pruritus, urticaria, and reactions suggestive of angioedema.
Cerebrovascular Adverse Reactions, Including Stroke: In clinical trials with antipsychotic drugs, elderly patients with dementia had a higher incidence of cerebrovascular adverse reactions, including fatalities, vs placebo. VRAYLAR is not approved for the treatment of patients with dementia-related psychosis.
Neuroleptic Malignant Syndrome (NMS): NMS, a potentially fatal symptom complex, has been reported with antipsychotic drugs. NMS may cause hyperpyrexia, muscle rigidity, delirium, and autonomic instability. Additional signs may include elevated creatine phosphokinase, myoglobinuria (rhabdomyolysis), and acute renal failure. Manage with immediate discontinuation, intensive symptomatic treatment, and monitoring.
Tardive Dyskinesia (TD): Risk of developing TD (a syndrome of potentially irreversible, involuntary, dyskinetic movements) and the likelihood it will become irreversible may increase with the duration of treatment and the cumulative dose. The syndrome can develop after a relatively brief treatment period, even at low doses, or after treatment discontinuation. If signs and symptoms of TD appear, drug discontinuation should be considered.
Late-Occurring Adverse Reactions: Adverse reactions may first appear several weeks after initiation of VRAYLAR, probably because plasma levels of cariprazine and its major metabolites accumulate over time. As a result, the incidence of adverse reactions in short-term trials may not reflect the rates after longer-term exposures. Monitor for adverse reactions, including extrapyramidal symptoms (EPS) or akathisia, and patient response for several weeks after starting VRAYLAR and after each dosage increase. Consider reducing the dose or discontinuing the drug.
Metabolic Changes: Atypical antipsychotics, including VRAYLAR, have caused metabolic changes, such as:
- Hyperglycemia and Diabetes Mellitus: Hyperglycemia, in some cases associated with ketoacidosis, hyperosmolar coma, or death, has been reported in patients treated with atypical antipsychotics. Assess fasting glucose before or soon after initiation of treatment, and monitor periodically during long-term treatment.
- Dyslipidemia: Atypical antipsychotics cause adverse alterations in lipids. Before or soon after starting an antipsychotic, obtain baseline fasting lipid profile and monitor periodically during treatment.
- Weight Gain: Weight gain has been observed with VRAYLAR. Monitor weight at baseline and frequently thereafter.
Leukopenia, Neutropenia, and Agranulocytosis: Leukopenia/neutropenia have been reported with antipsychotics, including VRAYLAR. Agranulocytosis (including fatal cases) has been reported with other antipsychotics. Monitor complete blood count in patients with pre-existing low white blood cell count (WBC)/absolute neutrophil count or history of drug-induced leukopenia/neutropenia. Discontinue VRAYLAR at the first sign of a clinically significant decline in WBC and in severely neutropenic patients.
Orthostatic Hypotension and Syncope: Atypical antipsychotics cause orthostatic hypotension and syncope, with the greatest risk during initial titration and with dose increases. Monitor orthostatic vital signs in patients predisposed to hypotension and in those with cardiovascular/cerebrovascular diseases.
Falls: VRAYLAR may cause somnolence, postural hypotension, motor and sensory instability, which may lead to falls and, consequently, fractures or other injuries. For patients with diseases, conditions, or medications that could exacerbate these effects, complete fall risk assessments when initiating antipsychotics and recurrently for patients on long-term therapy.
Seizures: Use VRAYLAR with caution in patients with a history of seizures or with conditions that lower the seizure threshold.
Potential for Cognitive and Motor Impairment: Somnolence was reported with VRAYLAR. Caution patients about performing activities requiring mental alertness (eg, operating hazardous machinery or a motor vehicle).
Body Temperature Dysregulation: Use VRAYLAR with caution in patients who may experience conditions that increase body temperature (eg, strenuous exercise, extreme heat, dehydration, or concomitant anticholinergics).
Dysphagia: Esophageal dysmotility and aspiration have been associated with antipsychotics. Antipsychotic drugs, including VRAYLAR, should be used cautiously in patients at risk for aspiration.
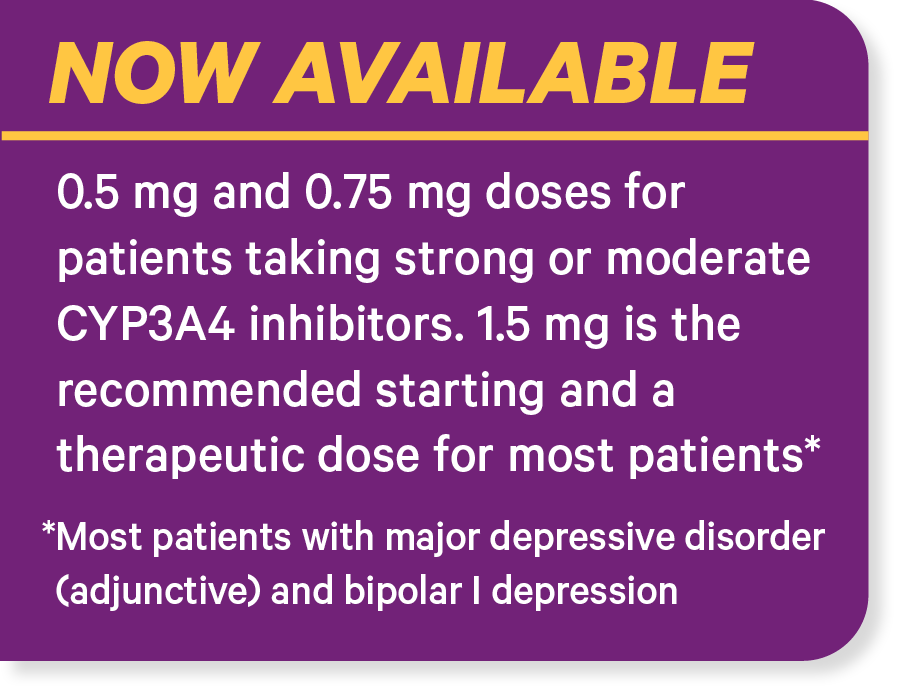
Drug Interactions: Strong and moderate CYP3A4 inhibitors increase VRAYLAR concentrations, so VRAYLAR dose reduction is recommended. Concomitant use with CYP3A4 inducers is not recommended.
Adverse Reactions: The most common adverse reactions in adult clinical trials (≥5% and at least twice the rate of placebo) are listed below:
- Adjunctive Treatment of Major Depressive Disorder:
- In 6-week, fixed-dose trials the incidences within the recommended doses (VRAYLAR 1.5 mg/day + antidepressant therapy [ADT] or 3 mg/day + ADT vs placebo + ADT) were akathisia (7%, 10% vs 2%), nausea (7%, 6% vs 3%), and insomnia (9%, 10% vs 5%).
- In one 8-week flexible-dose trial, incidences within the doses (VRAYLAR 1-2 mg/day + antidepressant therapy [ADT] or 2-4.5 mg/day + ADT vs placebo + ADT) were akathisia (8%, 23% vs 3%), restlessness (8%, 8% vs 3%), fatigue (7%, 10% vs 4%), constipation (2%, 5% vs 2%), nausea (7%, 13% vs 5%), increased appetite (2%, 5% vs 2%), dizziness (4%, 5% vs 2%), insomnia (14%, 16% vs 8%), and extrapyramidal symptoms (12%, 18% vs 5%).
- Bipolar Mania: The incidences within the recommended dose range (VRAYLAR 3–6 mg/day vs placebo) were EPS (26% vs 12%), akathisia (20% vs 5%), vomiting (10% vs 4%), dyspepsia (7% vs 4%), somnolence (7% vs 4%), and restlessness (7% vs 2%).
- Bipolar Depression: The incidences within the recommended doses (VRAYLAR 1.5 mg/day or 3 mg/day vs placebo) were nausea (7%, 7% vs 3%), akathisia (6%, 10% vs 2%), restlessness (2%, 7% vs 3%), and EPS (4%, 6% vs 2%).
- Schizophrenia: The incidences within the recommended dose range (VRAYLAR 1.5–3 mg/day and 4.5–6 mg/day vs placebo) were EPS (15%, 19% vs 8%) and akathisia (9%, 13% vs 4%).
VRAYLAR is available in 0.5 mg, 0.75 mg, 1.5 mg, 3 mg, 4.5 mg, and 6 mg capsules.
INDICATIONS AND USAGE
VRAYLAR (cariprazine) is indicated for adjunctive therapy to antidepressants for the treatment of major depressive disorder (MDD) in adults, for the treatment of depressive episodes associated with bipolar I disorder (bipolar depression) in adults, for the acute treatment of manic or mixed episodes associated with bipolar I disorder in adult and pediatric patients 10 years of age and older, and for the treatment of schizophrenia in adult and pediatric patients 13 years of age and older.
US-VRAA-250443